Sectional Matrices and the Restoration of Class II Direct Composite Restorations
Class II (interproximal) decay and/or a failing restoration that involves a posterior proximal surface is still a common finding in most dental patients. Many of these problems can be handled by using directly placed restorative materials. The challenge for the dentist always has been to create contact with the adjacent tooth and, at the same time, restore proper interproximal anatomic form given the limitations of conventional matrix systems. The thickness of the matrix band and the ability to compress the periodontal ligaments of the tooth being restored as well as the one adjacent to it can sometimes make the restoration of proximal tooth contact arduous at best.
THE MORPHOLOGY OF THE PROXIMAL SURFACE OF POSTERIOR TEETH
Anatomically, the posterior proximal surface is convex occlusally and concave gingivally. The proximal contact is elliptical in the buccolingual direction and located approximately 1 mm apical to the height of the marginal ridge. As the surface of the tooth progresses gingivally from the contact point toward the cementoenamel junction, a concavity exists that houses the interdental papilla. Conventional matrix systems are made of thin, flat metallic strips that are placed circumferentially around the tooth to be restored and affixed with some sort of retaining device. While contact with the adjacent tooth can be made with a circumferential matrix band, it is practically impossible to re-create the natural convex/concave anatomy of the posterior proximal surface because of the inherent limitations of these systems. Attempts to “shape” or “burnish” matrix bands with elliptical instrumentation may help create non-anatomic contact, but only “distorts” or “indents” the band and does not re-create complete natural interproximal contours. Without the support of tooth contour, the interdental papilla may not fill the gingival embrasure completely, leading to potential food traps and areas for excess plaque accumulation. Direct Class 2 composite restorations can present even more of a challenge to place for the dentist because of the inability of resin materials to be compressed against a matrix to the same degree as amalgam.
This article describes the use of an innovative sectional matrix system (Walser®,Vident, Brea, CA) and instrumentation designed to facilitate placement of these matrices to assure maximal results, both in physiologic contact and anatomic form. When using this system with the latest in composite resin technology, direct Class 2 tooth-coloured restorations can be placed that exhibit natural anatomic proximal form and have predictable proximal contact.1-3
TOOTH PREPARATION AND MATRIX ARMAMENTARIUM
Class 2 preparations that need a matrix band for restoration require rebuilding of the marginal ridge, proximal contact, and often a large portion of the interproximal surface. The goal with composite placement is to do so in a way that the amount of rotary instrumentation for contouring and finishing is limited. This is especially true for the interproximal surface. Because of the constraints of clinical access to the proximal area, it is extremely difficult to sculpt and contour this surface of the restoration correctly. Proper reconstruction of this surface is based largely on the shape of the matrix band and the accuracy of its placement.4
After removal of caries and old restorative material, the outline form of the cavity preparation is assessed. If any portion of the proximal contact remains, it does not necessarily need to be removed. As much healthy, unaffected tooth structure as possible should be conserved. If the matrix band cannot be positioned through the remaining contact easily, the contact can be lightened using a Gateway® 30-μm diamond strip (Brasseler USA, Savannah, GA).
A sectional matrix system, such as Walser, is an excellent choice for Class 2 composite restorations for many reasons. The matrix band is anatomically correct, and the unique design of the matrix allows for the proper restoration of interproximal anatomy as described. Also, the many matrix designs in the Walser system allow for accurate matrix fit for anterior Class 3 and 4 restorations, premolars, molars, and adjacent (back-to-back) proximal surfaces as well.
CASE REPORT: A CLASS 2 DIRECT COMPOSITE RESTORATION
The patient presented with an old Class 2 composite that had decay on the lingual aspect of the proximal portion of the restoration (Figure 1). After removal of the restorative material, associated decay, and preparation of the proximal cavity form, the operative area was isolated with a rubber dam (Figure 2). Notice the overcontoured proximal restoration in the adjacent tooth. This surface was recontoured and polished before placement of the matrix to create an ideal proximal contact for the restoration that is being placed (Figure 3).
The Walser sectional matrix system was chosen for this case to aid in the anatomic restoration of the mesial-proximal tooth morphology of this maxillary first premolar (Figure 4). The appropriate matrix band was chosen that best corresponded anatomically to the tooth being restored and also to the width and height of the proximal surface. The height of the sectional matrix should be no higher than the adjacent marginal ridge when properly placed. Because of the concave anatomic shape when applied, the proximal contact was located approximately 1mm apical to the height of the marginal ridge. Next, the gingival portion of the band was stabilized and sealed against the cavosurface margin of the preparation using the appropriate size FlexiWedge™ (Common Sense Dental Products, Inc, Spring Lake, MI). The size of the flexible wedge should be wide enough to hold the gingival portion of the matrix band sealed against the cavosurface of the preparation, while the opposite side of the wedge sits firmly against the adjacent tooth surface. If openings exist around the isolated teeth after rubber dam placement, a light-cured “liquid dam”(OraSeal® Ultradent Products, Inc, South Jordan, UT) can be used to seal the area(s) and prevent salivary contamination.
After the Walser matrix was properly wedged and in place, the restorative process began. A 15-second total-etch technique (10 seconds on enamel margins and 5 seconds on dentin surfaces) was performed using a 37% phosphoric etch (Figure 5). The etchant then was rinsed off for a minimum of 15 to 20 seconds to ensure complete removal (Figure 6). The preparation was then air-dried and rewet with Acqua Seal™ G desensitizer (Acqua-Med Technologies, Inc,West Chicago, IL) to disinfect the cavity surface, create a moist surface for bonding, and begin initial penetration of hydroxyethylmethacrylate (HEMA) into the dentinal tubules (Figure 7). A fifth-generation bonding agent (OptiBond® Solo Plus™, Kerr Corporation, Orange, CA) then was placed on all cavity surfaces (Figure 8). The solvent was evaporated by spraying a gentle stream of air across the surface of the preparation. The adhesive was light-cured for 20 seconds.
The first layer of composite was placed using a flowable composite (Beautifil® Flow F10, Shofu Dental Corp, San Marcos, CA) to a thickness of about 0.5 mm (Figure 9). The flowable composite “flowed” into all the irregular areas of the preparation and created an oxygen-inhibited layer to bond subsequent layers of microhybrid material. After light-curing for 20 seconds, the next step was to layer the microhybrid composite material. First, using a unidose delivery, the first increment of composite resin (Beautifil® II, Shofu Dental Corp) was placed into the proximal box of the preparation. Beautifil II is described by the manufacturer as “a nano-hybrid composite with fluoride release and recharge.” A smooth-ended condensing instrument (Goldstein Flexi-Thin Mini 4, Hu-Friedy, Chicago, IL) was used to adapt the restorative material to the inside of the sectional matrix and preparation.
A contact-forming instrument, such as the Trimax™ composite instrument (AdDent Inc, Danbury, CT), can be used to aid in the creation of a “composite bridge” to hold the matrix against the adjacent tooth and to create a proximal contact, if necessary (Figure 10). Each increment of composite material should be no more than 2 mm thick. The buccal increment was placed into the facial portion of the preparation (Figure 11), including the facial portion of the marginal ridge. The cuspal projections were sculpted and the depressions between were created using the FlexiThin Mini 4. A No. 2 Flat Keystone brush (Patterson Dental, St. Paul, MN) was dipped lightly in resin, dried thoroughly with a 2 in x 2 in sponge, and used to feather the material toward the margins (Figure 12) and smooth the surface of the composite.
The palatinal increment of microhybrid composite (Beautifil II) was placed in the same manner as previously described (Figure 13 and Figure 14). After completion of the composite placement and before matrix removal, the restoration was lightcured using an LED curing light (Translux Power Blue™, Heraeus Kulzer, Inc, Armonk, NY) (Figure 15 and Figure 16).
The occlusion was checked with articulation paper after removal of the rubber dam and adjusted as needed using a needle-shaped composite finishing diamond (Brasseler USA). When placing composite materials using the described technique, very little finishing should be required, except at the marginal areas. Rubber polishing abrasives were used to polish the adjusted areas. After a 5-second etch of the restorative margins with 37% phosphoric acid (Figure 17), the surface sealant (ClearCheck SLP, Shofu Dental Corp) was placed with the No. 2 Flat Keystone brush, air-thinned, and lightcured for 20 seconds.
Surface sealants help to seal microscopic marginal imperfections that may remain after the finishing and polishing process. Figure 18 shows an occlusal view of the completed Class 2 composite restoration. Notice the beautiful chameleon effect that was achieved using one shade of composite (Beautifil II) and how well the restorative material blends with the adjacent tooth structure.5,6
CONCLUSION
A technique has been described using a sectional matrix system (Walser) and associated armamentarium and a nanofilled microhybrid composite (Beautifil II) to create an anatomically precise Class 2 posterior composite restoration. The interproximal surface was re-created with natural anatomic contour and elliptical contact with the adjacent tooth. With proper occlusal and proximal form, this “invisible” direct composite restoration will service the patient for many years to come.7

Figure 1 Preoperative occlusal view of tooth No. 5, which had recurrent caries in the lingualproximal area of a 10-year-old composite resin restoration.

Figure 2 After isolation, the defective restoration was removed, and the preparation was modified to remove the recurrent caries. Note the overcontouring of the composite restoration in tooth No. 4 and how this helped to create a concavity in the distoproximal of the restoration (see Figure 1) that is now to be replaced on tooth No. 5.

Figure 3 An ET® 3 (Brasseler USA) was used to contour the adjacent restoration before the placement of the matrix on tooth No. 5.

Figure 4 Using placement forceps, the Walser matrix (No. 6 for small bicuspid) was placed around the prepared tooth. If the matrix does not easily slip through the proximal area, lighten the contact with a 30-μm diamond strip. A flexible wedge helped seal the gingival floor of the proximal box tightly against the cavosurface margin.

Figure 5 A total-etch technique was used with a 15-second total-etch time of enamel and dentin. Start with the application of etchant on the enamel only, then continue to dentin, which requires only 5 seconds of etching.

Figure 6 The etchant was rinsed for at least 15 seconds (a longer rinse time can be used). Then, the preparation was air-dried thoroughly, removing all moisture.

Figure 7 A desensitizer was placed to rewet the enamel and dentin surfaces and gain initial penetration of HEMA and fluoride into the dentinal tubules to aid in formation of the hybrid zone.

Figure 8 A fifth-generation adhesive (OptiBond Solo Plus) was applied copiously to the enamel and dentinal surfaces.

Figure 9 A thin layer of flowable composite (Beautifil Flow F10) was placed no thicker than 0.5 mm then, using an explorer tip, was spread to cover the dentin and fill all the geometric line and point angles of the restoration. The goal was to create a uniformly thin layer of resin in intimate contact with the cured adhesive, eliminating the possibility for voids between the composite and adhesive layer. Also, on curing, the oxygen-inhibited layer will form a sticky surface onto which the successive layers of composite resin will be adapted more easily with less chance of “pull back.”

Figure 10 A composite-contact forming instrument (Trimax composite instrument) was used to help push the matrix and adapt the composite firmly against the adjacent proximal surface. The composite then was cured in place, forming a “composite bridge” that guarantees a strong contact on removal of the matrix.

Figure 11 A FlexiThin Mini 4 was used to place the facial increment of composite (Beautifil II) in the preparation.

Figure 12 A No. 2 Flat Keystone brush was used to smooth and adapt the composite to the marginal area. This will help to reduce the amount of rotary finishing needed.

Figure 13 With the facial increment placed and sculpted, the lingual increment is about to be placed.

Figure 14 The FlexiThin Mini 4 was used to sculpt the lingual (palatal) surface of the restoration.
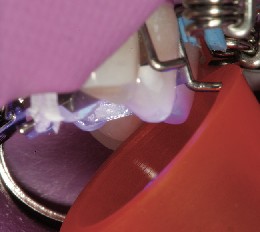
Figure 15 The lingual increment was lightcured for 30 seconds.

Figure 16 Occlusal view of the completed restoration before removal of the matrix and finishing procedures were performed.

Figure 17 After checking occlusion, adjusting where necessary, finishing, and polishing the restoration, a 5-second etch was performed to clean the marginal area, then copiously rinsed with water and air-dried.

Figure 18 Occlusal view of the completed restoration after light-curing of the surface sealant.
Robert A. Lowe, DDS
Diplomate
American Board of Aesthetic Dentistry
Charlotte, North Carolina USA
REFERENCES
1. Christensen GJ. Remaining challenges with class II resin-based composite restorations. J Am Dent Assoc. 2007;138(11): 1487-1489.
2. Boer WM. Simple guidelines for aesthetic success with composite resin—part 2: posterior restorations. Pract Proced Aesthet Dent. 2007;19(4):243-247.
3. Shuman I. Excellence in class II direct composite restorations. Dent Today. 2007;26(4): 102-105.
4. Brackett MG, Contreras S, Contreras R, et al. Restoration of proximal contact in direct class II composites. Oper Dent. 2006;31(1):155-156.
5. Lopes GC, Vieira LC, Araujo E. Direct composite resin restorations: a review of some clinical procedures to achieve predictable results in posterior teeth. J Esthet Restor Dent. 2004;16(1):19-32.
6. Lowe RA. Recreating nature using today’s composite materials. Restorative Quarterly. 2000;3(1):3-10.
7. Lowe RA. Morphologic and esthetic precision in the placement of class II direct composites. Contemporary Esthetics and Restorative Practice. 2004;8(5):28-30.




